Human procreation means sexual reproduction resulting in human fertilization, usually due to sexual intercourse between a male and a female.
To ensure a successful fertilization both the man and the woman must have adequate levels of fertility.
Although there are many medical practitioners treating female infertility, let alone the treatment, knowledge of male infertility itself is obscure among the general public.
In an insightful interview, one of the handful of male infertility specialists in the whole of South Asia, Dr. Rohana Priya Susantha Ranasinghe sheds some light about this lesser known topic and dispels several myths that are deep-rooted in our society.
Q: What is infertility?
A: Infertility is the inability of a person, animal or plant to procreate by natural means.
It is normally not the natural state of a healthy adult and in humans, infertility is the inability to become pregnant or carry a pregnancy to full term.
The interaction between the two opposite reproductive systems during sexual intercourse results in fertilization of the female eggs by the sperm.
The World Health Organization defines ‘infertility’ as “a disease of the reproductive system defined by the failure to achieve a clinical pregnancy after 12 months or more of regular unprotected sexual intercourse.
Primary infertility is infertility in a couple who have never had a child. Secondary infertility is failure to conceive following a previous pregnancy.
Infertility may be caused by infections, ailments or diseases in the man or woman, but often there is no obvious underlying cause.
Most medical practitioners consider failure to cause pregnancy within one year as a likelihood of ‘mild infertility’.
We don’t necessarily call it a situation of mild infertility but subject the patients to fertility tests.
Mild infertility is also dependent on age of the couple.
If the patients are 25 years of age or below, it is standard to wait and see for two years.
But if they are around 30 years, period of one year in waiting is usually the norm and this is reduced to just six months if the couple is 35 or above.
Q: There is lot of talk about female infertility among the general public, but many feel that there is inadequate awareness about male fertility among the general public. Doctor, what exactly is male infertility?
A: Male infertility refers to a male's inability to cause pregnancy in a fertile female.
Although people do not want to accept the magnitude of the problem due to cultural stigma and gender connotations, it is a worldwide medical condition now.
Although in 1971, only five per cent of total world population suffered from mild infertility, by 2012 this figure has trebled to 15% due to various social, environmental and dietary factors.
Various studies have found out that males and females contribute equally or roughly 40% each to mild infertility, where as the balance causes for 20% of the cases are categorized as ‘unexplained’.
As I mentioned earlier, infertility is not always primary which means that the patients are unable to have their first baby but also secondary, tertiary etc unable to have their second child after having their first.
Q: How do you diagnose mild male factor infertility (MMFI) and what are the causes for MMFI?
A: Mild male factor infertility is where the capability of male patient’s sperm to cause pregnancy is lower than the average male.
There are three main causes for mild male factor infertility.
1.) Lower sperm count (Quantitative)- The minimum sperm count accepted as a norm by medical practitioners is 15 million sperms in 1 milliliter of semen
2.) Lower motility - Sperm motility is the movement and swimming of the spermatozoa. Poor sperm motility means that the sperm is unable to move properly. Poor sperm motility is also called asthenozoospermia.
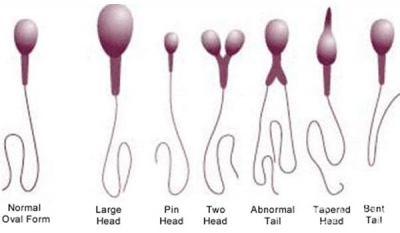
3.) Abnormal sperm morphology - sperm morphology means the shape or physical appearance of sperm. Abnormalities in the sperm morphology can lead to failure in causing pregnancy resulting in infertility.
But although as you said people are somewhat more aware of female infertility and there is lot of discussion about it, male infertility has become a taboo subject and as a result there is hardly any discourse about it as unlike their female counterparts, males who suffer from male infertility or mild male factor infertility to be exact, do not wish to talk about it.
But mild male factor infertility is not a big deal now.
Anyone can do a simple sperm fertility test at any accredited laboratory and find results on his own.
My message is don’t fear infertility and just in case you have mild male factor infertility, there is treatment available in Sri Lanka.
Q: If the patient is suffering from mild male factor infertility, what are medical options available for him?
A: Unfortunately, there are no universally accepted treatments for mild male factor infertility in modern medicine, except for the Ayurvedic treatment which we have developed through research.
This is similar to paralysis where there is no treatment currently to cure paralysis, except in Ayurveda.
If a patient is suffering from mild male factor infertility, he has no option but to seek assisted reproduction technologies.
However in a country like Sri Lanka medical costs are comparatively higher (in comparison to income of an average citizen).
In vitro fertilization (IVF) or popularly known as the test tube baby method are out of the reach of ordinary citizens while even the simple Intrauterine insemination (IUI) also has a significant cost.
Q: So are these procedures helpful in treating mild male factor infertility?
A: Yes that is problem. Although these can help patients for whom normal or natural fertilization would be problematic these are still assisted reproduction technologies and not treatments.
The problem is although these are costly methods the success rates still could be lower.
In such instances, male infertility treatments can greatly enhance the success rates of these procedures.
Unfortunately forget people in the Western world lot of Asians including Sri Lankans think that male factor infertility cannot be treated and don’t know that Ayurveda can successfully treat male factor infertility.
Q: So do you think our society is adequately aware of infertility?
A: Unfortunately no. There are many factors that impair the reproductive system’s ability to perform the basic function of reproduction.
Although conceiving a child sounds like a simple and natural process, the internal and physiological functions are quite complex and sophisticated and depend on many factors.
So patients must know that production of healthy sperm by the male, production of healthy ovum by the female, unhindered access to the sperm to reach the ovum in ampulla in the fallopian tubes, the sperm's capability to successfully fertilize the ovum, the ability of the zygote (fertilized egg) to bind successfully in the endometrium of the uterus and finally the ability of the zygote to achieve adequate embryo quality.
Although we have achieved many advancements, modern medicine has very little means to improve sperm count on one hand and motility and morphology of the sperm on the other hand and as a result mitigation of male infertility is in most cases unsatisfactory in my view.
However Ayurvedic medicine offer a greater proportion in our society a significant improvement in sperm quality and quantity and our studies have continuously proven that herbal-based Ayurvedic treatments promote the production of healthy sperm.
(Dr. R.A.R.P. Susantha Ranasinghe [PhD, D.S.A.M.S., B.A.C.(Pg.D.), M.A.B.A.C.] is an outstanding Ayurvedic physician and researcher who championed the cause of traditional and hereditary knowledge of herbal medicine especially in the treatment of infertility. He can be contacted on This email address is being protected from spambots. You need JavaScript enabled to view it.)
Captions
1.) Sperms swimming towards an egg (Image courtesy- conceiveplease.com )
2.) Healthy female reproductive system (Image courtesy- anatomyparts.us )
3.) Normal and abnormal sperms (Image courtesy- ehealthcares.info )
4.) Healthy male reproductive system (Image courtesy- anatomyparts.us )
5.) Female egg and the male sperm fuse to create a zygote cell which then turns into an embryo. 23 chromosomes from the male and female each.